Human Cord Blood Stem Cell Differentiates into Lung Cell
29 Dec, 2006 03:23 pm
Human umbilical cord blood (UCB) stem cell research shows great promise, especially as we continue to learn more about the differentiation capabilities of these stem cells. During the past few years, researchers have determined cord blood includes cells capable of turning into cell types representative of all three germinal layers (e.g., endoderm, ectoderm and mesoderm). These early stage cell layers give rise to the body?s more complex tissues and organs. For example, the endoderm layer produces our gastrointestinal and respiratory tracts, as well as endocrine glands and organs, such as the thyroid and pancreas. The few research groups reporting success in differentiating cord blood stem cells into all three layers have confirmed endodermal potential by turning them into liver cells [1,2].
Our research further demonstrates the endodermal potential of human UCB-derived stem cells to serve as highly functional tools for studying lung pathophysiology in a human model instead of primary culture/animal models. We hope to translate this early research success into future breakthroughs that ultimately provide therapeutic benefits to patients suffering from lung injuries and respiratory conditions.
Additional Cytotherapy Study Details
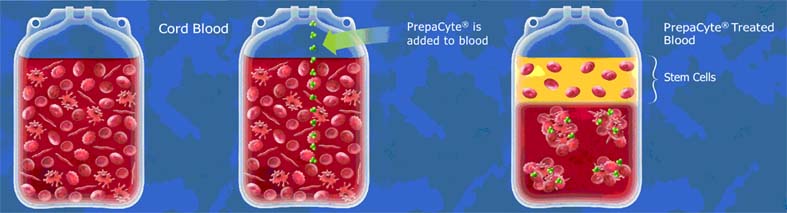
To obtain the MLPC from cord blood, we used a stem cell isolation technology — PrepaCyte-MLPC — from BioE. We successfully isolated the rare MLPC from four UCB units obtained from the American Red Cross (Cord Blood Program, St. Paul, Minn., USA) (Fig. 1).
We then put the UCB stem cells into culture and allowed them to expand using mesenchymal stromal cell growth medium (MSCGM) prior to adding small airway growth medium (SAGM), both mediums from Cambrex BioScience (East Rutherford, N.J., USA). Following several days in culture, we demonstrated differentiation of MLPCs into type II alveolar cells, which was confirmed by the presence of a definitive type II alveolar cell marker — surfactant protein C (SPC).
Impact and Next Steps
Researchers have derived respiratory epithelial cells — including type II alveolar cells — from murine embryonic and marrow stem cells and human embryonic stem cells (ESCs) [4,5,6]. However, to the best of our knowledge, this is the first time human, non-embryonic, multi-potent stem cells have turned into type II alveolar cells. Aside from the current multi-faceted debate surrounding the use of ESCs, prominently in the United States, this development is significant for a number of reasons.
First, early work to differentiate human and murine ESCs into alveolar cells has been limited with differentiation rates of approximately two percent of human ESCs in culture [6] to nearly undetectable levels with mouse ESCs [7]. However, we were able to successfully induce essentially all MLPCs into type II alveolar cells.
Second, alveolarization — or the transformation of immature, saccular lung to mature lung with developed alveoli able to facilitate gas exchange — begins at approximately 36 weeks of gestation and continues through the first few postnatal years. The relatively late occurrence of the alveolarization process in fetal development is why some premature babies are born with underdeveloped lungs. (It’s estimated only 15 percent of alveoli are formed at birth [8].) As a result, it is plausible UCB is a more optimal source of stem cells than ESCs for creating alveolar cells. However, research has yet to fully prove this point.
In the future, the MLPC could be used as a research tool to better understand lung development and disease. For example, we may be able to examine cord blood from babies who have lung diseases, such as cystic fibrosis, to determine how these conditions evolve and to develop better medical treatments. Type II alveolar cells derived from the MLPC also may be useful to test potential new drugs that could aid in combating diseases such as emphysema, as well as pulmonary injury due to therapy-related causes.
BioE funded and participated in our original study. We have since entered into another joint research collaboration with the company to further evaluate the use of its MLPC for creating airway epithelial cells — such as type II alveolar cells — for research and therapeutic applications. This research is expected to conclude in mid-2008.
References:
(1) Lee OK, Kuo TK, Chen WM et al. Isolation of multipotent mesenchymal stem cells from umbilical cord blood. Blood. 2004; 103: 1669-75.
(2) Kogler G, Sensken S, Airey J et al. A new human somatic stem cell from placental cord blood with intrinsic pluripotent differentiation potential. J Exp Med. 2004; 200: 123-35.
(3) Berger MJ, Adams SD, McKenna DH et al. Differentiation of umbilical cord blood-derived multilineage progenitor cells into respiratory epithelial cells. Cytotherapy. 2006; 8: 480-87.
(4) Ali N, Edgar AJ, Samadikuchaksaraei A et al. Derivation of type II alveolar epithelial cells from murine embryonic stem cells. Tissue Eng. 2002; 8: 541-50.
(5) Panoskaltsis-Mortari A, Hermanson J, Price A et al. Differentiation of type II pneumocyte-like cells from murine bone marrow derived multipotent adult progenitor cells (MAPCs) in vitro. American Thoracic Society International Conference. Am J Respir Crit Care Med. 2004; 169 (Suppl): A87.
(6) Samadikuchaksaraei A, Cohen S, Isaac K et al. Derivation of distal airway epithelium from human embryonic stem cells. Tissue Eng. 2006; 12: 867-75.
(7) Rippon H, Polak J, Qin M, Bishop A. Derivation of distal lung epithelial progenitors from murine embryonic stem cells using a novel 3-step differentiation protocol. Stem Cells. 2006; 24: 1389-98.
(8) Merkus P, ten Have-Opbroek A, Quanjer P. Human lung growth: a review. Pediatr Pulmonol.1996; 21: 383-97.
David McKenna, M.D. is an assistant professor of lab medicine and pathology and medical director of the University of Minnesota Medical Center, Fairview’s Clinical Cell Therapy Lab, and principal investigator of Cytotherapy study in the article.






